Article by Bradley Fowler, Forté Healthcare – October 2021.
This document has been produced by Forté Healthcare for the exclusive use of the recipient and may not be copied or reproduced without appropriate references and the express permission of the author.
The heels are one of the most susceptible sites for pressure injuries, due to factors such as heel anatomy, disease burden, comorbid conditions, and the aging process[1],[2]. Heel Pressure Injuries (HPI) have been found to be one of the most prevalent sites for pressure injuries to occur, with a study in Europe identifying that 38.5% of stage IV pressure injuries were found at the heels[3]. Pressure upon the Calcaneus can be reduced and redistributed by elevating the lower leg and calf 2. There are three primary designs of heel elevation discussed in this article: the Heel Slope (Surface Modification), Heel elevator (external device) and the elevated Heel slope (Hybrid Model).
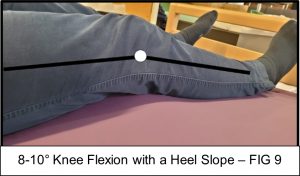
Though essential in the clinical setting, and particularly with those that are medically complex 2, elevating the heel and redistributing the pressure towards the calf is a difficult task. There are several implementation considerations such as ensuring the knee is at a slight flexion (5-10°) while the heel is elevated can help avoid vein compression and increased risk of deep vein thrombosis[4] (DVT), adapting a plan of care to the individuals’ needs and avoiding causing harm to other ‘at-risk’ areas of the body (such as the Achilles tendon) 2.
With patients on a traditional support surface with a completely horizontal fascia (no heel slope), and no additional aid from an external heel device [FIG 1], pressure injuries upon the heel region are more common than with heels that have elevated heels[5],[6],[7] with differences being from an 8% to 54.2% incidence on heel injury respectively 6.
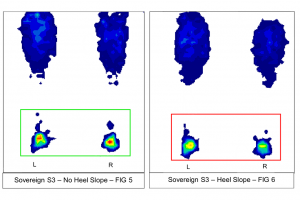
Forté Healthcare have conducted studies into the effects of heel elevation between a Non-Heel Slope [FIG 1], Heel Slope [FIG 2], Heel Elevator [FIG 3] and the Elevated Heel Slope [FIG 4]. For purposes of this article, however, results are shown of the Heel Slope and Non-Heel Slope to show illustrate the basic principles of heel elevation.
Using a Tekscan Pressure Measurement System which utilises a thin and flexible sensor. We use this system to measure the pressure distribution of a human body on the surface of our mattresses with minimal interference.
The images below demonstrate the pressure distribution of the NPIAP/RESNA 50th Percentile male mannequin[8] [FIG 8] (81.2kg, 1775mm tall) as over a 6-hour period, shown in a variety of heel positions. The Support surface used is a Single Sovereign S3 High-Care Mattress.
Note:
- The mannequin is a rigid model. Results are not a reflection of the human body dynamics, however, are used as an illustration of the physical aspects to Heel Elevation.
- Pressure Mapping is a commonly used tool in attaining clinical data on interface pressures, however Forté Healthcare acknowledges “it cannot be used to conclude on internal stresses and the stress concentration levels in deep vascularized tissues, particularly muscles”[9].
- The example pressure mapping provided by Forté Healthcare is only intended for use as a clinical aid, “rather than a replacement to clinical judgement”[10]
As observed both qualitatively and quantitatively, the Support Surface with a heel slope immediately reveals as significantly more effective at offloading pressure from the Heels. Between the heel sloped Surface and no heel slope, the Peak pressures upon the heel region reached a percentage difference in Pressure of 50.6% [GRAPH 1].
Such a decrease in pressure, therefore, signifies the importance of heel offloading, and indirectly the importance of utilising a support surface modified with a heel slope as a means of offloading such pressure and reducing risk of an HPI. Furthermore, the heel slope was identified to encourage a slight bend in the knee of approximately 8-10°, in comparison to a flat surface which evidence has suggested reduces popliteal vein compression4.

[1] Delmore B, Lebovits S, Suggs B, Rolnitzky L, Ayello EA. Risk factors associated with heel pressure ulcers in hospitalized patients. J Wound Ostomy Continence Nurs. 2015 May-Jun;42(3):242-8; quiz E1-2. doi: 10.1097/WON.0000000000000134. PMID: 25945823.
[2] European Pressure Ulcer Advisory Panel, National Pressure Injury Panel and Pan Pacific Pressure Injury Alliance. Prevention and Treatment of pressure injuries; clinical Practice Guideline. The International Guideline. Emily Haesler (Ed.) EPUAP/NPIAP/PPPIA: 2019
[3] Vanderwee K, Clark M, Dealey C, Gunningberg L, Defloor T. Pressure ulcer prevalence in Europe: a pilot study. J Eval Clin Pract. 2007 Apr;13(2):227-35. doi: 10.1111/j.1365-2753.2006.00684.x. PMID: 17378869.
[4] Huber DE, Huber JP. Popliteal vein compression under general anaesthesia. EUR J Vasc Endovasc Surg, 2009; 37(4); 464-469.
[5] Bååth C, Engström M, Gunningberg L, Muntlin Athlin Å. Prevention of heel pressure ulcers among older patients–from ambulance care to hospital discharge: A multi-centre randomized controlled trial. Appl Nurs Res. 2016 May;30:170-5. doi: 10.1016/j.apnr.2015.10.003. Epub 2015 Oct 26. PMID: 27091274.
[6] Donnelly J, Winder J, Kernohan WG, Stevenson M. An RCT to determine the effect of a heel elevation device in pressure ulcer prevention post-hip fracture. J Wound Care. 2011 Jul;20(7):309-12, 314-8. doi: 10.12968/jowc.2011.20.7.309. PMID: 21841719.
[7] Cadue JF, Karolewicz S, Tardy C, Barrault C, Robert R, Pourrat O. Efficacité de supports anatomiques en mousse pour la prévention des escarres de talons. Etude contrôlée randomisée en réanimation médicale [Prevention of heel pressure sores with a foam body-support device. A randomized controlled trial in a medical intensive care unit]. Presse Med. 2008 Jan;37(1 Pt 1):30-6. French. doi: 10.1016/j.lpm.2007.07.009. Epub 2007 Nov 26. PMID: 18037257.
[8] RESNA (2019). American National Standard for Support Surfaces – Volume 1: Requirements and Test Methods for Full Body Support Surfaces (ANSI/RESNA SS-1:2019). 2019
[9] A. Gefen & J. Levine (2007) The false premise in measuring body-support interface pressures for preventing serious pressure ulcers, Journal of Medical Engineering & Technology, 31:5, 375-380, DOI: 10.1080/03091900601165256
[10] Dunk AM & Gardner A (2016) Body shape: a predictor for pressure injury risk, Wound Practice and Research, 24:2, 92-98, ISSN 2202-9729